In our last installment, we discussed the problems and issues with Biofilm in the wound care space today. We looked at the molecular physiology and the formation MMPs or metalloproteases as well as the alteration of fibroblasts and peripheral keratinocytes. But in order to really understand why Biofilm colonizes wounds, we must clearly understand the formation of a Chronic Wound and how and why it develops.
Chronic Wounds are wounds that can not advance beyond the inflammatory process in the wound healing stages and do not follow the normal wound healing sequence. This usually leads to a lot of pain and discomfort over time as well as comorbidity, infection, amputation and sometimes even death. Chronic wounds present an enormous challenge moving into the future and the reason I mention this is from prior studies within the literature indicating rising costs and social economical burdens.
So, how does a chronic wound develop? Is it due to a wound that is neglected or uncared for? Or perhaps does a chronic wound develop if the wound becomes infected? To delineate the actual mechanism of why a chronic wound develops, I will carefully walk you through the physiology of what we call Redox Biology. I first became interested in Redox Biology several years ago while battling some challenging cases. Sharp debridement had always served me well along with continued daily topical treatments of various antibiotic ointments and enzymatic applications. I wound also combine multi-modal sequencing of different wound care modalities as dictated by the presentation of the wound in a holistic approach. Most of the time this also included a multi-disciplinary team concept ensuring that there was vascular integrity, infection control, and an understanding of the etiology of the wound coupled with labs, radiological studies, antibiosis, and off-loading measures.
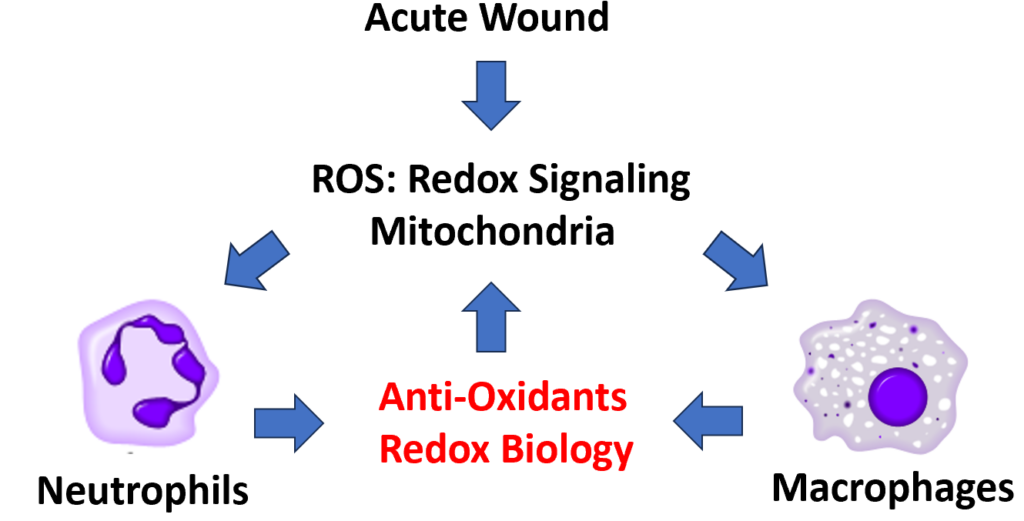
In order to understand why a chronic wound develops, we will first look at what happens physiologically to the acute wound. When a wound first develops, the mitochondria first begin a signaling sequence. This signal is what we call ROS or Reactive Oxygen Species. The mitochondria are the work horse of the cell and release ROS from the metabolization of oxygen molecules. The ROS particles are basically free radicals and include H202 (hydrogen peroxide), OH (Hydroxyl anions), and variations of O2 or oxygen radicals. The ROS then signal two very important cells to the wound site: Neutrophils and Macrophages which engulf bacteria via a process known as phagocytosis. In turn, the neutrophils and macrophages then release what are known as Anti-oxidant particles. This is called Redox Biology. The anti-oxidants as the name implies, neutralizes the ROS particles or free radicals and maintains a tight regulatory control on the free radicals (see picture below).
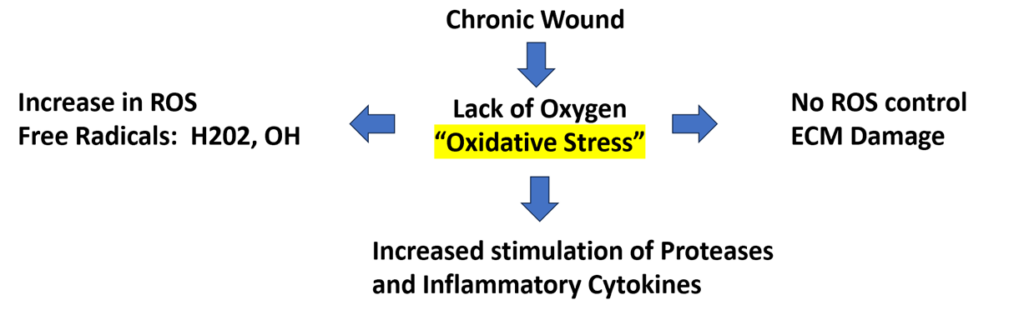
However, in a chronic wound, the ROS or Reactive Oxygen Species are not under the tight regulatory control of the anti-oxidants and therefore become rogue. As the acute wound begins to become oxygen deprived due to the surface tension of the wound (lack of debridement and surface tissue slough), Oxidative Stress then develops which has a domino effect throughout the physiological process. As a result of oxidative stress or increased wound tension across the surface of the wound, ROS particles begin to increase which then results in damage to the ECM or extracellular matrix. With damage and destruction to the ECM, the neutrophils and macrophages become altered as well as the fibroblasts and keratinocytes. This ultimately results in the impaired release of anti-oxidants leading to further damage internally. Therefore, there is an increased stimulation of the proteases and inflammatory cytokines within the cellular matrix. The defense host protective systems then break down at the surface of the wound which then lead to the formation of microbial colonization known as Biofilm.
In my next installment of wound bed preparation and the fight against Biofilm, we will continue our discussion and look at literature-based evidence on sharp debridement as well as innovative methodology in creating better wound trajectories in the treatment of chronic wounds. Please check back often and until next time, fair winds and following sees.
Cheers,
Dr. F. Derk


