Per our recent discussion on Bacterial Fluorescence Imaging as a Predictor of Skin Graft Integration, I would also like to share another slide demonstrating the importance of eradication of Bacterial Fluorescence or Bioburden/Biofilm. The prior article consisted of Split Thickness Skin Grafts and their survival rate based on the eradication of bacterial fluorescence or the presence of bioburden/biofilm. With eradication, the study demonstrated significant results in graft survival rates and aligns with wound bed preparation. In fact, it is wound bed preparation that is the foundation to sharp debridement in order to eradicate biofilm. Yes, it is true that there are topical agents which will kill surface biofilm, however, biofilm is layered and studies have shown that biofilm can survive below the wound itself. Therefore, it is the action of sharp debridement which will disrupt the layers of tissue slough, devitalized tissue, and colonies of bioburden throughout the wound bed. However, the means by which we sharply debride can vary as with the use of scapels and curettes which have been adopted into the wound care space. With curettes, the depth of debridement can vary with the slightest of angulation and pressure as well as the clinician’s acumen and experience level. With variations as such, often times bleeding results especially in those patients who are on anticoagulants not to mention the pain patients may experience especially if there is unintentional deep penetration.
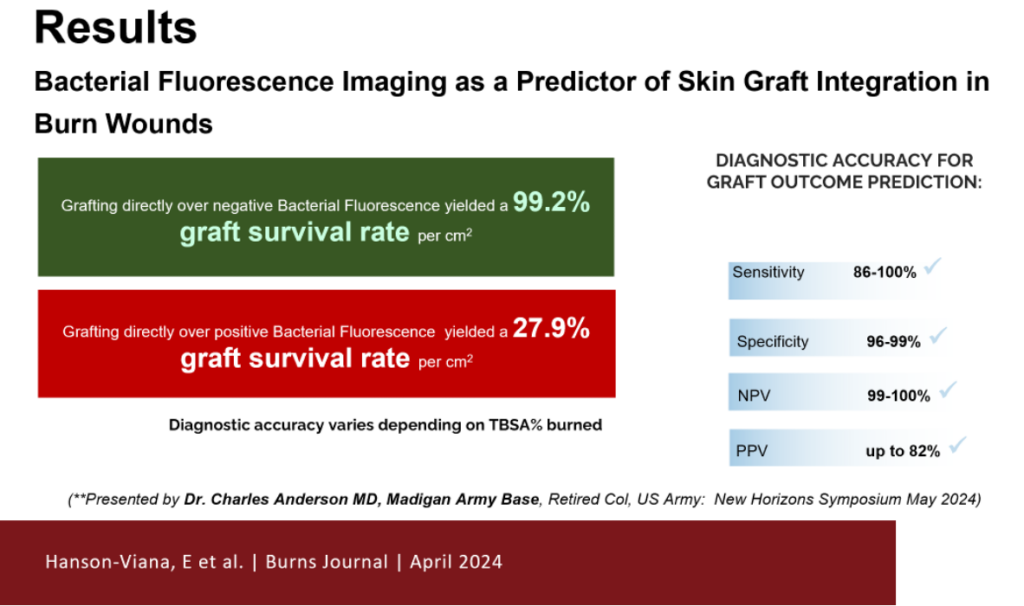
The slide above demonstrates a significant reduction in the wound size with the eradication or reduction of Bacterial Fluorescence (Biofilm) with a decrease in wound area by 28% per week. And an increase in the wound size without the eradication or reduction of Bacterial Fluorescence (Biofilm) by 7% per week. In essence, the removal of biofilm as demonstrated in both studies using fluorescence scanning not only allowed for a greater survival rate for grafts, but also revealed a decrease in the size of the wound. This also aligns with Nusbaum’s study which revealed sharp debridement weekly favors wound healing by 43%!
As we move forward in best wound care practices, Biofilm is becoming the talk of the town and this is very evident by a profound shift in the way we are now concentrating efforts on wound bed informatics. While attending a conference last year, it was not surprising to see a majority of vendors sporting their skin substitutes. What was very surprising however was the large number of vendors introducing hypochlorous acid and copolymer products for the application of killing biofilm. I also had the opportunity to speak to several vendors and simply asked if their products were the best in the eradication of biofilm. One particular vendor skirted the issue for several minutes and then finally concluded that sharp debridement was necessary as did the others. Don’t get me wrong, I honestly feel that such products are extremely useful, but the gold standard for wound bed disruption and biofilm eradication is sharp debridement by which many other products can work in concert to ultimately produce better outcomes. Bottom Line Up Front (BLUF): As we are becoming more familiar with Biofilm and producing feasible means of identifying it, the next natural progression will be to eliminate it. All roads are leading to the eradication of biofilm in my humble opinion and the next progression will be how will we do that effectively, accurately with repeatable and reproducible results without the complications usually encountered with surgical instrumentation including bleeding and pain. And that is where the story of EZDebride fills that void.
